Frequently Asked Questions and Troubleshooting
Frequently Asked Questions
-
Why is nutrition important in Motor Neuron Disease?
Getting enough nutrition helps the body to function. Energy (also called kilojoules or calories) and protein from food and drink can help slow down muscle loss and help reduce tiredness, fight infections and assist with wound healing.
-
Is it my decision to have a gastrostomy feeding tube?
Yes. It is your decision to have a gastrostomy feeding tube. It is important to know that your decisions and views will be respected and your healthcare team will provide support with either decision.
-
Can I still eat and drink if I have a gastrostomy feeding tube?
Yes. A gastrostomy feeding tube does not prevent you from eating or drinking. Some people have a gastrostomy tube placed before they even need to use it. Others eat and drink normally for enjoyment and use the gastrostomy tube to ‘top up’ their nutrition and fluids. Your Dietitian will work with you to decide how much food and fluid you need through your gastrostomy tube. Your Speech Pathologist will suggest safe swallowing techniques to help you eat and drink safely through your mouth.
-
Will a gastrostomy feeding tube extend my life?
Unfortunately, Motor Neuron Disease will still progress whether you decide to have a gastrostomy tube or not, however research evidence indicates that gastrostomy feeding in Motor Neuron Disease may extend people’s lives by some months and may improve quality of life.
-
Can it become too late to have a gastrostomy feeding tube inserted?
Unfortunately, yes. The biggest factor impacting your ability to have a gastrostomy tube is your lung function. If your breathing muscles are too weak, you will not be able to tolerate the sedation given for the procedure. Some people decide to have a PEG tube placed early, before they need to start using the tube to make the procedure as safe as possible.
-
Can I change my mind after the gastrostomy feeding tube is inserted?
Yes. You can change your mind if you want to remove the gastrostomy tube after discussion with your medical team. This depends on factors such as your lung function and ability to swallow. Your medical team can talk you through procedures for removing your gastrostomy feeding tube.
-
What will happen if I choose not to have a gastrostomy feeding tube?
If you choose not to have a gastrostomy feeding tube it may become harder to meet your nutrition and hydration needs. Your healthcare team will work with you to use strategies to maintain your ability to eat and drink for as long as possible. When the time comes where you can no longer safely eat or drink, the palliative care team will help with comfort and symptom management. It is best to speak to your healthcare team about this.
-
Can I bath and shower normally with a gastrostomy feeding tube?
Yes. It is recommended for the first two weeks to shower only. After two weeks, is it acceptable to have a bath. When bathing make sure the tube is capped shut beforehand and dry the tube and exit site carefully with a soft towel afterward.
-
Can I go swimming with my gastrostomy feeding tube?
Yes. It is recommended to avoid swimming for the first 6 weeks to allow the site to heal. After 6 weeks, it is perfectly safe to go swimming so long as the tube is capped shut beforehand and dried carefully afterwards.
-
Will my bowels be affected with a gastrostomy feeding tube?
Many people with Motor Neuron Disease have trouble with their bowels. This may be due to weakness of the muscles that help pass bowel movements, or not getting enough fibre and fluids (helps soften the stool) due to swallowing difficulties. If you find you are having trouble with your bowels after starting tube feeds, your Dietitian may recommend you switch to a feed that has added fibre or your doctor may prescribe you some medication.
-
How do I get feeds and equipment for my gastrostomy feeding tube?
Your Dietitian will enrol you in a Home Enteral Nutrition Program where you will receive a monthly delivery of feeds and/or equipment. It is easy to change or cancel orders over the phone. If you attend the Motor Neurone Disease Clinic at Flinders Medical Centre and you have a Gastrostomy tube placed in a public hospital, then you will be eligible for free feed and equipment. However, if you have your Gastrostomy tube placed privately, then you may not qualify for free feeds/equipment. If you are aged under 65 years, you may also qualify for NDIS funding. Speak to your Dietitian for more information.
-
What happens if my tube falls out?
Don’t panic, however it is important to act quickly because the exit site will quickly start to close over. A well-established tract can close over within 12-24 hours. If your tube becomes accidently dislodged call for an ambulance (000) or present immediately to your nearest emergency department.
Deciding on a Gastrostomy Feeding Tube
Living with a gastrostomy feeding tube
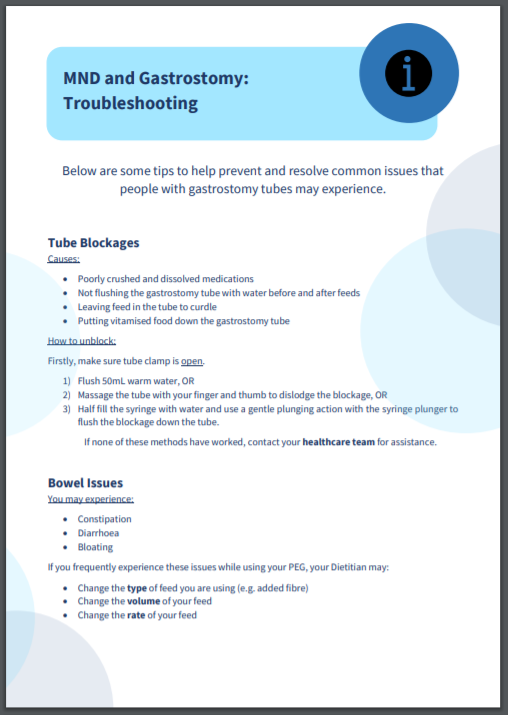
Troubleshooting
Click to view our printable troubleshooting list.

Click here to listen to Dr Allcroft discussing the issue of constipation (7 minute video)
-
Gastrostomy Feeding Tube
A small, flexible tube that is inserted into the abdominal wall of the stomach to allow nutrition, hydration and certain medications to be given.
-
Bolus Feed
A set amount of feed given through the tube, usually mimicking breakfast, lunch, dinner and/or mid meals. A ‘bolus’ refers to one “meal” of feed formula.
-
Continuous Feed
Liquid feeds are given by a feeding pump at a slow feeding rate. Continuous feeds can occur during the day or overnight, depending on the individual.
-
Flushing
The administration of water down the tube for cleaning and to prevent blockages.
-
Clamp
A plastic stopper that prevents liquids flowing back our of the tube when flushing, feeding or giving medications.
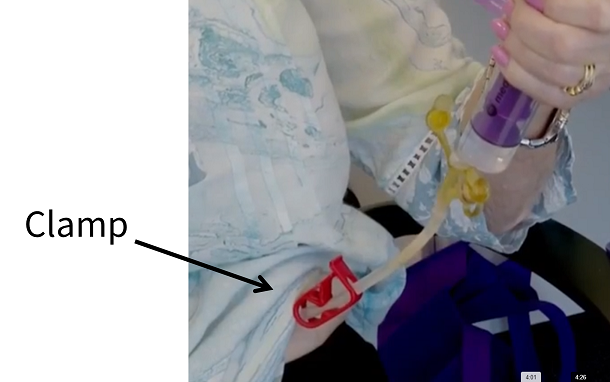
During Feeding:
• Keep the clamp closed while you are preparing liquids to flush down the tube (e.g. using the plunger to draw up feeds
• Open the clamp when you are putting liquids down the tube
• Close the clamp for 30 minutes after flushing/ giving feeds /medications to prevent backflow of liquids.
After feeding:
• Open the clamp 30 minutes after flushing/ giving feeds /medications and keep the clamp open until next use to prevent damage to the tube. -
PEG (Percutaneous Endoscopic Gastrostomy)
A feeding tube that is fitted with anaesthetic by a Gastroenterologist and is placed directly into the stomach.
-
RIG (Radiological Inserted Gastrostomy)
A feeding tube that is fitted with anaesthetic by the X-Ray Department and is placed directly into the stomach. This is a different method for those with poor lung function.
-
Feeding Pump
A machine that gives the feed through the Gastrostomy feeding tube into the stomach.
-
Giving Set
Plastic tubing that allows feed to move through the tube with a feeding pump. One end of the tube joins to the bag of feed and one joins to the Gastrostomy feeding tube.
-
Syringe
A plastic tube and plunger used to push feed through the tube. This type of syringe is called a catheter syringe and does not have a needle.
-
Aspiration
A condition when food, liquids, saliva or vomit enters the lungs.
-
Choking
Occurs when the airway is blocked by food or liquids
-
Dysphagia
Impaired swallowing.
Glossary
Further Information
- Motor Neurone Disease Australia: Information on scientific research related to Gastrostomy Tube Feeding.
https://www.mndcare.net.au/Living-with-MND/Symptom-management/Swallowing/Maintaining-nutrition/Gastrostomy-(PEG-and-RIG).aspx - Motor Neurone Disease Association of New South Wales: Information on considering Gastrostomy – PEG and Rig.
https://www.mndnsw.asn.au/about-mnd/information/153-managing-with-mnd/living-better/234-considering-gastrostomy-peg-and-rig-eb8.html - Leeds NHS Trust: Video guide to looking after and using a PEG tube.
https://www.youtube.com/watch?v=bKEgSlszEx0 - Anna Penhall’s story
https://www.youtube.com/watch?v=dWgrNzGBPEc
Acknowledgements
We would like to acknowledge the fantastic contribution made by the following:
- The patients and families involved from the SA State-wide MND Clinic
- Tom Buring – Telerehab ICT Administrator, Division of Rehabilitation, Aged Care and Palliative Care
- MND Clinic multidisciplinary team – Flinders Medical Centre, Division of Rehabilitation, Aged Care and Palliative Care
- Dietetic Department – Flinders Medical Centre, Division of Rehabilitation, Aged Care and Palliative Care
- Amy Brown – Student dietitian from Flinders University (2020)
- Nikita Wilson-Beddoe – Student dietitian from Flinders University (2019)
- Kaye Bevan
For further Information or general enquiries please contact:
Liz Kapur – Dietitian, Division of Rehabilitation, Aged Care and Palliative Care
Email: elizabeth.kapur@sa.gov.au
Special mentions to the individuals who feature in the application.
Patients:
- Wendy
- Anton
- Jodie
- Darryl
- Jill
- Graham and partner Barb
- Peter and partner Polly
- Anna and partner Scott
- Karen and partner Gordon
- Bill and partner Keryn
- Chris and partner Samantha
- Genevieve
Clinicians:
- Dr Charles Cock – Gastroenterologist
- Dr Peter Allcroft – Palliative Care Physician
- Liz Kapur – Dietitian
- Megan Hide – Speech Pathologist
- Dr Karin Myhill - Psychiatrist
Page 6 of 6